Managing Antimicrobial Resistance Without On-Site Specialists
Modern diagnostics are everywhere, but infectious disease expertise is not, leaving community hospitals to make high-stakes decisions without a specialist in the room.

In the halls of major academic medical centers, Antimicrobial Stewardship Programs (ASPs) are robust machines. Teams of Infectious Disease (ID) pharmacists and physicians rotate pagers, reviewing every request for meropenem or piperacillin-tazobactam. They have the infrastructure, the manpower, and the budget to police antibiotic use effectively.
But what happens in the community hospital down the road? Or the skilled nursing facility (SNF) in a rural county?
According to studies, 80% of counties in the United States don't even have access to an infectious disease doctor. (https://doi.org/10.7326/M20-2684)
We are facing a crisis of access. In this environment, superbugs are thriving, and hospitals are facing an "Expertise Gap" that threatens both patient safety and the bottom line.
The "Haves" and the "Have-Nots"
In Prescribe Responsibly, Episode 1, Dr. Zachary Mostel highlights the stark operational contrast between academic theory and community reality. "ASPs are effective, but they require a ton of infrastructure and manpower to implement them effectively," he notes. "You usually see them at large academic centers and not so much at community hospitals."
This is the Stewardship Gap.
In an academic center, an alert regarding a multi-drug resistant organism (MDRO) triggers a cascade of expert interventions. In a community hospital, that same alert often lands on the desk of a general hospitalist managing a high patient census. These providers often lack the time, and the specific genomic training, to decode the nuances of a complex molecular panel.
The result is an operational blind spot that compromises patient safety and drains hospital budgets.
The lack of onsite Infectious Disease (ID) expertise creates downstream effects that negatively impact hospital margins through three specific mechanisms:
1. The Operational Cost of Therapeutic Lag
In the absence of an ID expert to interpret advanced molecular diagnostics (PCR), generalists often revert to the "wait and see" approach, relying on traditional cultures.
While modern lab technology can detect a pathogen in hours, the clinical decision is frequently delayed by 48 to 72 hours while waiting for culture results. This "Therapeutic Lag", the time between patient presentation and the start of optimal therapy, represents a massive inefficiency. The hospital pays for rapid diagnostics but fails to realize the ROI because the expertise to interpret the data immediately is unavailable.
- Operational Impact: Every day a patient sits in this decision lag is an avoidable increase in Length of Stay (LOS).
- Clinical Impact: For septic patients, mortality risk increases significantly for every hour effective antibiotic therapy is delayed.
2. The Price of Defensive Prescribing
When a physician is unsure if a specific resistance marker is relevant to the patient's current condition, they prescribe out of fear. Dr. Mostel notes that doctors "fear essentially doing nothing for the patient," leading to defensive prescribing.
A patient with a complex UTI might receive multiple high-cost antibiotics (e.g., vancomycin and cefepime) not because they definitely need them, but because the provider lacks the confidence to de-escalate. Without a specialist to authorize a "narrower" therapy, such as ceftriaxone or ampicillin-sulbactam, these expensive drugs often run for the duration of the admission.
This drives two negative outcomes:
- Pharmacy Bloat: Unnecessary consumption of high-cost agents.
- Compliance Risk: Prolonged broad-spectrum use is a primary driver of C. diff infections—a Hospital-Acquired Condition (HAC) that carries significant CMS penalties.
3. The Revolving Door of Readmissions
As Dr. Mostel points out, resistant infections require precise management. If a community provider attempts to treat a resistant infection with a standard antibiotic because they did not recognize a specific marker on the lab report, the therapy will fail.
Dr. Mostel notes that for these resistant cases, patients "often do not have oral options for antibiotic therapy" and require intravenous (IV) intervention. However, without expert guidance, a generalist may attempt an oral course hoping to avoid a complex discharge.
The patient may show temporary improvement, but the infection persists. This creates a revolving door effect: the patient is discharged, only to return to the ER days later, often septic and requiring ICU admission.
For the administrator, this triggers CMS Readmission Penalties. For the facility, it represents a failure to leverage existing data. The diagnostic report contained the answer, but the "Expertise Gap" prevented the translation of that data into a cure.
Scaling the Expert Mind
We cannot clone Dr. Mostel. We cannot manufacture enough ID physicians to staff every rural hospital in America overnight. But we can scale their decision-making logic.
This is the core premise of Arkstone’s OneChoice®.
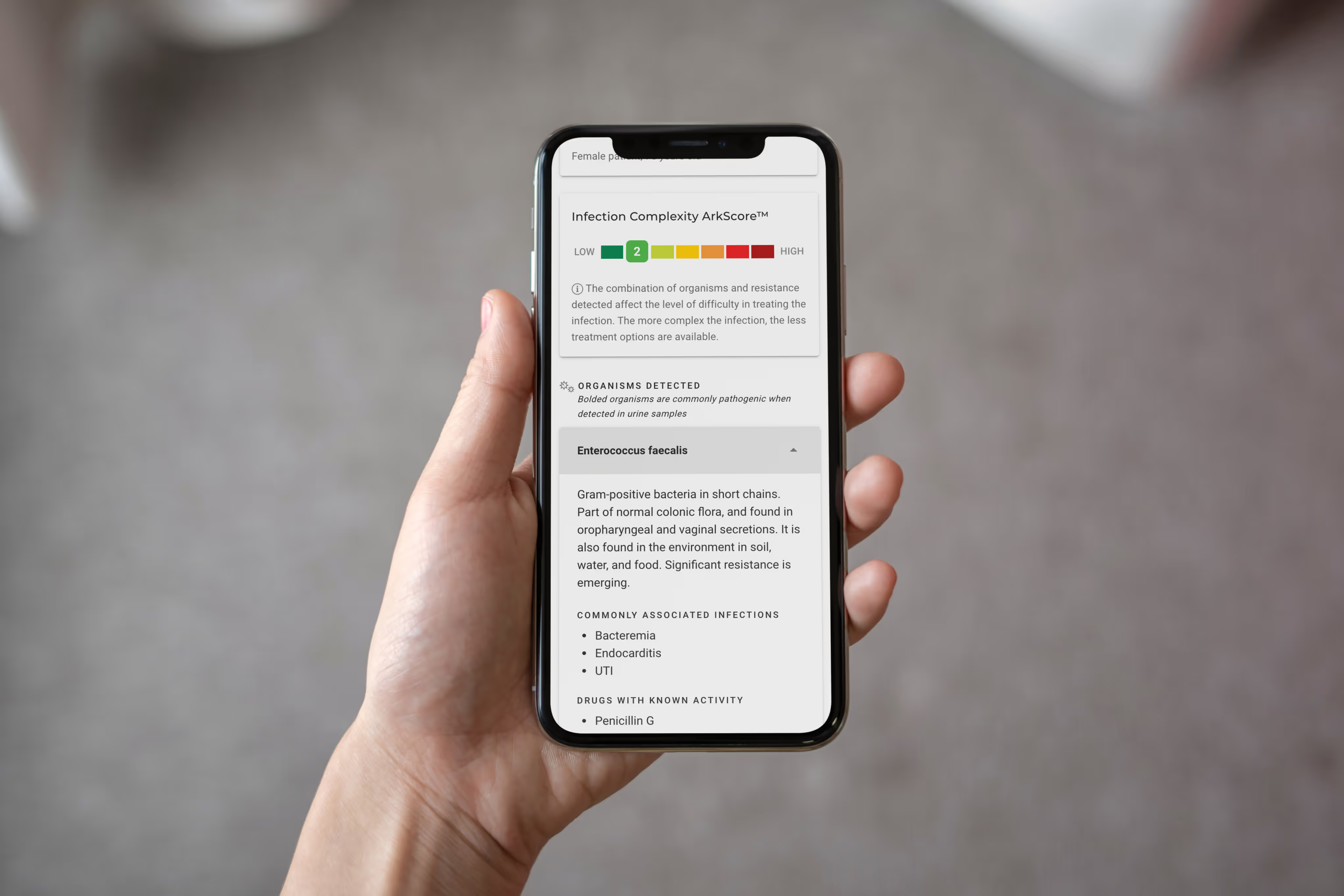
Imagine if every lab report came with a digital ID consult attached. Instead of just listing "Pathogen Detected" and a confusing table of resistance genes, the report utilizes Arkstone’s decision engine to synthesize the data exactly as Dr. Mostel describes.
- Interpretation: Multi-drug resistant organism detected.
- Clinical Context: Patient lacks viable oral options (analyzed via OneChoice® logic).
- Guidance: Intravenous therapy required; standard oral prophylaxis is contraindicated.
This technology bridges the gap between the raw data provided by modern molecular diagnostics and the clinical application required at the bedside. It effectively exports the "brain" of an ID specialist into the 80% of counties that lack one.
From Vendor to Partner
For the laboratory, Arkstone is a massive differentiator. In a commoditized market where every lab offers the same PCR panels, the lab that offers Arkstone’s OneChoice® wins the account. The lab becomes a partner in patient care, not just a vendor of results.
For the hospital administrator, this is a cost-saving mechanism. By integrating Arkstone’s OneChoice®, the facility reduces Length of Stay by getting the patient on the right drug on Day 1, not Day 4. It reduces the burden on the few ID consultants they might have, allowing them to focus on the most critical cases rather than routine stewardship reviews.
Conclusion
The "Expertise Gap" is a choice. We have the technology to irrigate these regions with high-quality clinical decision support. As the AMR threat grows, relying on generalists to guess their way through complex resistance patterns is no longer a viable strategy. It’s time to bring the expert to the bedside, digitally.
Share this article
Blogs
Latest Blogs
Stay informed with our featured blogs.
Customer Testimonials
Arkstone's solutions have transformed our patient care.
Take the Next Step, Try OneChoice®
No more guesswork. No more lookup tools. No more inaccuracies and inconsistencies. No more stopping to ask for directions.